In addition to expanding Medicaid and reducing the number of uninsured, the Affordable Care Act (ACA) included a number of initiatives to expand already existent coordinated care models including Accountable Care Organizations (ACOs) and Patient Centered Medical Homes (PCMH). An additional incentive program, omnipresent in US health policy discussions at the moment, the Delivery System Reform Incentive Payment Project (DSRIP) is a pay for performance incentive with a twofold goal: 1) to reduce avoidable hospitalizations and 2) to lower overall health care spending. While not required by the program, linking DSRIP’s Medicaid reform incentives with the ACO and PCMH approaches, typically separated from Medicaid, can benefit both hospital centers and patients.
The DSRIP program hopes to incentivize infamously stagnant hospital systems into changing the way they do business, placing patient outcomes and cost control at the center of their motivation, rather than profit maximization. The Kaiser Commission on Medicaid and the Uninsured summarizes DSRIP as a partnership between federal and state governments to help hospitals achieve the “triple aim†goals of health reform as defined by the Institute for Healthcare Improvement: to improve population health, the patient experience, and reduce the per capita cost of care.
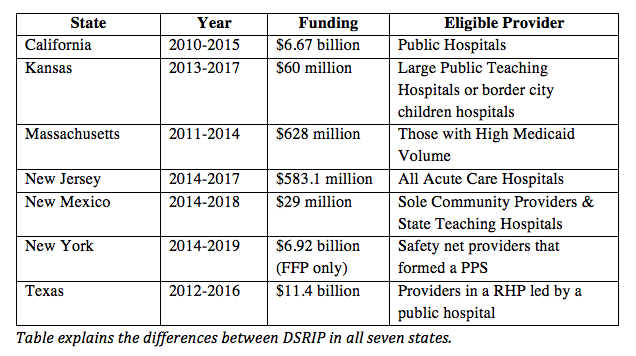
The National Association of Medicaid Directors summarizes the participating states’ DSRIP programs and, along with the Kaiser Commission report, explains that each state has the flexibility to innovate within their existing Medicaid programs. As the table demonstrates, every state has widely varied approaches and financing. This effort can be further improved by incorporating models originally targeting private insurance patients, also incentivized under the ACA, most importantly, ACOs.
The table illustrates that New York (NY) and New Jersey (NJ) have different eligibility requirements than the other states, since health care in NY and NJ is more complex and competitive. As the Schuyler Center for Analysis and Advocacy summarized, to receive full compensation in New York, only safety net hospitals and physician groups, those that treat a large volume of Medicaid patients, are invited to form a community-wide partnership, known as a preferred provider system (PPS). The PPS is responsible for all care in a designated geographic region, and those that incorporate a PCMH approach into their DSRIP system can receive a higher “DSRIP score,†which means more Medicaid reimbursement revenue.
Across the river in NJ, all acute care hospitals can participate in DSRIP. However, despite many major health systems in NJ having an ACO, the ACO model is rarely integrated with the state’s DSRIP program. Under the DSRIP program in NJ, each hospital chooses to focus on a specific chronic disease and provides the full continuum of care to those patients. This is very similar to an ACO approach, which provides incentives for full continuum patient-centered care, and the state could benefit from further alignment. By integrating existing ACOs with DSRIP, hospitals can better provide this coordinated care model and could receive more in reimbursements, since in an ACO, the ACO entity shares any cost savings with the insurer thus adding to more revenue for the care providers.
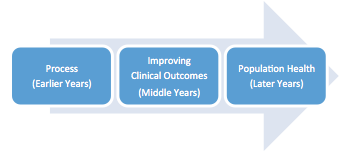
DSRIP programs link the specific project milestones to reimbursements in an aim to achieve complete Medicaid transformation (defined by the “triple aimâ€). Initial projects tend to be simpler and deal with infrastructure and system development such as meeting health IT integration “meaningful use†or implementing telemedicine (process projects). Later projects are likely to be more complicated, and include creating a full continuum of care for a patient with HIV/Aids (population health). These later projects can often involve utilizing a PCMH or ACO model.
The DSRIP proposal allows every participating entity within the state to design a DSRIP program that fits with their specific patient demographics. The PCMH and ACO approaches are proven to help hospitals and providers to coordinate care and by integrating with DSRIP will help hospitals and providers achieve DSRIP metrics and receive more reimbursements. Thus, patients can be at the center of the healthcare spectrum and can receive the best possible treatment creating better and safer hospitals.
Daniel B. Shulkin is a Masters of Public Administration Candidate in Health Policy and Management at the Robert F. Wagner Graduate School of Public Service of New York University. He is also a Health Finance and Outcomes Research Fellow at the Greater New York Hospital Association (GNYHA).
Disclaimer: Any views or opinions presented in this Op-Ed are solely those of the author and do not necessarily represent those of GNYHA.